Cancer remains one of the most formidable health challenges worldwide, impacting millions of people and claiming countless lives every year. Despite decades of research and advances in treatment options, cancer continues to be a leading cause of death across the globe. Its complex nature, variety of forms, and ability to resist conventional therapies make it a daunting opponent for scientists and healthcare professionals alike.
Yet, with medical science progressing faster than ever before, innovative developments are emerging that hold promise in this ongoing struggle. The development of cancer-preventing or -fighting vaccines is one of the most thrilling and promising advancements. These vaccines signify a strategic change, transitioning from solely addressing cancer post-appearance to preventing its onset altogether or aiding the immune system in fighting existing tumors. This evolution in healthcare mirrors similar holistic approaches seen in other areas of wellness, such as those detailed in Eddie Abbew’s diet plan, nutrition tips, and fitness secrets, where prevention and proactive health management take center stage.
Among these pioneering innovations, the first cancer vaccine is notable as a transformative milestone. It heralds a new age in cancer prevention and therapy, paving the way for opportunities that were previously considered unfeasible. It is vital for all parties involved, including patients, caregivers, health advocates, and policy makers, to grasp the workings of this vaccine, its recommended recipients, and its efficacy.
This detailed article will explore the realm of the first cancer vaccine in depth. We will discuss all the essential aspects: the scientific principles of how it functions, the individuals who stand to gain the most from it, its demonstrated safety and efficacy, and the promising advancements in cancer vaccines. This guide aims to inform, inspire, and empower, whether you’re looking to learn for yourself or to help spread awareness.
What Is a Cancer Vaccine?
In order to grasp the importance of the first cancer vaccine, one must comprehend what a cancer vaccine truly is. Vaccines are biological agents that prepare the immune system to identify and fight off pathogens, usually viruses or bacteria. With regard to cancer, though, the principle is a bit more complicated.
Cancer vaccines can be divided into two primary categories: preventive and therapeutic vaccines. The goal of preventive cancer vaccines is to prevent the initial development of cancer by targeting known carcinogenic viruses or factors. In contrast, therapeutic vaccines aim to assist the immune system in combating existing cancer.
The crucial element of a cancer vaccine is to provoke the immune system to identify cancer cells as threats and assault them. In contrast to conventional vaccines that guard against infectious diseases, cancer vaccines serve two purposes: they either prevent cancers associated with viruses or assist in treating existing cancers by focusing on specific tumor markers.
History of Cancer Vaccines
For decades, scientists have been fascinated by the idea of using the immune system to combat cancer. At the beginning of the 20th century, scientists observed that infections could sometimes lead to tumor reduction, which generated interest in cancer treatments based on the immune system. It was only in the late 20th century that substantial advancements were achieved in the development of vaccines aimed specifically at cancer.
Among the research milestones was the identification of oncogenic viruses, which can lead to cancer, including the Human Papillomavirus (HPV) and Hepatitis B Virus (HBV). These findings opened the door for vaccines that avert infections resulting in cancer. These vaccines were supported by rigorous clinical trials and research conducted by prominent institutions around the globe.
The First Cancer Vaccine: What Is It?
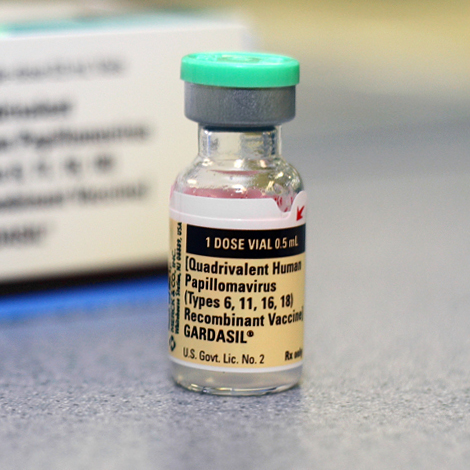
The HPV vaccine, marketed under brand names like Gardasil and Cervarix, is the first cancer vaccine to gain widespread recognition and FDA approval. This vaccine, which was approved in the mid-2000s, targets particular strains of HPV that are accountable for most cervical cancer cases and other cancers such as anal, throat, and penile cancers.
The HPV vaccine functions by presenting the body with benign proteins from the virus, thereby conditioning the immune system to identify and eliminate HPV should it attempt to infect cells. The vaccine effectively lowers the risk of developing cancers linked to HPV by preventing HPV infection.
Another significant cancer vaccine is the Hepatitis B vaccine, which aids in preventing liver cancer linked to chronic HBV infection. These vaccines, when combined, constitute the inaugural class of cancer vaccines that have had a considerable effect on global cancer prevention.
Who Should Get the First Cancer Vaccine?
The HPV vaccine is primarily recommended for preteens, usually aged 9 to 12, before they begin sexual activity. Vaccination guidelines, however, differ among health organizations. Many recommend vaccination until age 26, and some consider adults up to 45 eligible for vaccination after consulting their healthcare provider.
It is crucial for those who are at increased risk of exposure to or infection with HPV to receive the vaccine. It is important to note that vaccination against other strains can benefit even those who have already been exposed to one strain of HPV.
Likewise, it is advisable for newborns, healthcare professionals, and those at increased risk of HBV infection to receive the Hepatitis B vaccine. The two vaccines are vital public health instruments designed to avert viral infections that cause cancer.
Effectiveness and Safety of the Vaccine
Extensive clinical trials and real-world data have demonstrated the success of the HPV and Hepatitis B vaccines. For instance, the HPV vaccine has demonstrated a significant reduction in cervical cancer rates in countries where vaccination programs are widespread. Research shows that there is a considerable decrease in HPV infections and precancerous cervical lesions in populations that have been vaccinated.
Any vaccine must prioritize safety, and the cancer vaccine is no different. The vaccines for HPV and Hepatitis B have undergone thorough testing and monitoring. Generally, side effects are mild and can include soreness at the injection site, a slight fever, or headaches. Severe adverse effects occur very infrequently.
Even though their safety and effectiveness are established, myths and misunderstandings regarding these vaccines continue to spread. To make informed choices, it is crucial to depend on trustworthy scientific data and the guidance of health authorities.
The Impact of the First Cancer Vaccine on Cancer Treatment and Prevention
The advent of the first cancer vaccine has revolutionized cancer prevention. For many years, the emphasis was primarily on early identification and management. Vaccines now provide the opportunity to completely prevent the development of certain cancers.
Countries where vaccination rates are high have documented drops in cervical cancer incidence, showcasing a significant public health achievement. Additionally, these vaccines have motivated the investigation of therapeutic vaccines for various other types of cancer.
Also, cancer vaccines signify a move toward immunotherapy—treatments that utilize the immune system to combat cancer. This method works alongside established treatments such as chemotherapy and radiation, providing patients with new hope.
Future of Cancer Vaccines
The initial cancer vaccine is designed for cancers linked to viruses, but current studies seek to broaden the application of vaccine technology to other non-viral cancer types. Researchers are developing personalized cancer vaccines that tailor immune responses according to an individual’s tumor profile.
The development of these next-generation vaccines is being hastened by progress in genomics and immunology. Vaccines aimed at melanoma, lung cancer, prostate cancer, and other conditions are currently being tested in clinical trials.
Challenges persist, such as the intricate nature of cancer biology and the necessity for strong immune activation that does not produce adverse effects. There are also ethical issues, including the accessibility of vaccines and their fair global distribution.
How to Stay Informed and Take Action
Increasing awareness is essential to optimizing the advantages of cancer vaccinations. If people do not know the necessity of these life-saving vaccines or do not know when and how to get vaccinated, then simply having access to them is insufficient. To guarantee that vaccines have the full protective impact, immunization regimens must be followed in accordance with public health recommendations. Furthermore, routine cancer screenings support immunization efforts by identifying any early illness indicators, which can greatly enhance treatment results.
It is crucial for parents to have an honest and knowledgeable discussion with clinicians regarding vaccination their children against Hepatitis B and HPV. When given before to viral exposure, usually in early adolescence, these vaccinations work best. To guarantee that their children receive timely protection, pediatricians can answer any questions, offer the most recent advice, and help parents with the immunization procedure.
Adults should actively discuss immunization alternatives with their healthcare professionals. People in high-risk categories, such as those with weakened immune systems or specific lifestyle choices that make them more susceptible to HPV or Hepatitis B infections, should pay particular attention to this. Depending on each person’s health and risk profile, medical professionals can provide tailored advice and choose the most effective immunization plan.
Relying on reliable and authoritative sources is crucial for staying informed and making educated health decisions. Reputable institutions that frequently update recommendations and offer educational materials regarding cancer vaccines include the World Health Organization (WHO), the Centers for Disease Control and Prevention (CDC), and national cancer institutes. Having access to reliable information from these sources aids in debunking myths and false information that could otherwise deter vaccination. In the end, being aware encourages proactive health decisions that safeguard entire communities as well as individuals.
An enormous accomplishment in both public health and medical science is the first cancer vaccine. These vaccinations have the potential to save millions of lives and drastically lower the worldwide cancer burden by preventing infections that cause cancer.
The prospect of a time when many malignancies can be prevented or successfully treated increases as research and new vaccines are developed. People who are knowledgeable about the facts, advantages, and suggestions pertaining to cancer vaccines are better equipped to advocate for increased vaccine accessibility and make wise health decisions.
Since prevention is always preferable to cure, take action right now by becoming more knowledgeable about cancer vaccinations and promoting immunization in your community.
People Also Ask About the Cancer Vaccine
Q1: What is the first cancer vaccine and how does it work?
The first cancer vaccine is the HPV vaccine, which protects against human papillomavirus infections that can lead to cervical and other cancers. It works by training the immune system to recognize and destroy HPV before it causes harm.
Q2: Who should get the cancer vaccine?
The cancer vaccine is recommended primarily for preteens aged 9 to 12 but can be given up to age 26 or older depending on individual circumstances. Both boys and girls should receive the vaccine to maximize protection.
Q3: Is the cancer vaccine safe?
Yes, the cancer vaccines like HPV and Hepatitis B have been extensively tested and monitored. They are considered very safe with only mild, temporary side effects such as soreness or mild fever.
Q4: Can the cancer vaccine prevent all types of cancer?
No, current cancer vaccines prevent specific cancers caused by viruses, such as cervical and liver cancer. Research continues to develop vaccines for other cancer types.
Q5: Where can I get the cancer vaccine?
Cancer vaccines are available at clinics, hospitals, and public health centers. Speak to your healthcare provider to learn about vaccine availability and schedules near you.
Cancer prevention starts with knowledge and proactive steps. If you or your family members haven’t yet received the cancer vaccine, now is the time to talk to your healthcare provider about scheduling it. The HPV and Hepatitis B vaccines have already saved countless lives, and by getting vaccinated, you join a global effort to reduce the burden of cancer.
Share this article from quicknewsfeed.com with your friends and family to help spread awareness about the first cancer vaccine and why it matters. The more people understand and act, the closer we get to a future where cancer is no longer a leading threat.
Stay informed, stay protected — and help us make cancer prevention a priority worldwide. For more up-to-date health news and vital information, keep visiting quicknewsfeed.com.